Rising global temperatures tied to rising antibiotic resistance
A new data analysis suggests that two rising public health threats — climate change and antibiotic resistance — are related. The study, spanning 2000 to 2016, doesn’t establish cause and effect. But its findings, in the journal Eurosurveillance, suggest that rising global temperatures could be helping to fuel increases in antibiotic-resistant bacteria.
Key takeaway
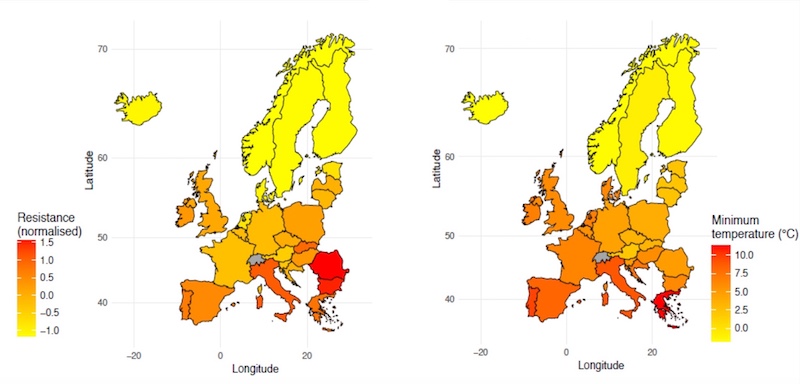
Countries with warmer minimum temperatures recorded a more rapid rise in the prevalence of antibiotic resistance from 2000 to 2016.
Researchers led by Mauricio Santillana, PhD, and Sarah McGough, PhD, in the Boston Children’s Hospital Computational Health Informatics Program (CHIP) tapped national surveillance data from 28 European countries, incorporating test results from more than 4 million patients. They analyzed the prevalence of antibiotic resistance over time, focusing on three common bacteria (Escherichia coli, Klebsiella pneumoniae, and Staphylococcus aureus). They also gathered European temperature data from European and U.S. sources.
“Our longitudinal study is the first to show that European countries with warmer ambient minimum temperature have had more acute increases in antibiotic resistance over the last 17 years,” says Santillana, who is also affiliated with Harvard Medical School and the Harvard T.H. Chan School of Public Health. “This observation helps explain the geographic differences in antibiotic resistance documented in other cross-sectional studies. Such resistance could eventually render our most effective antibiotic agents obsolete.“
Temperatures and antibiotic resistance rise in synch
Southern European countries with minimum temperatures that were 10°C (18° F) warmer — like Spain, Portugal, Romania, and Italy — recorded a more rapid rise in the prevalence of antibiotic resistance over time than cooler Northern European countries like Sweden, Finland, and Norway. The increases in resistance ranged from 0.33 to 1.2 percent per year, even after accounting for factors like local population density and local patterns use of antibiotic use.
The association held for all four antibiotic classes analyzed, and for two of the three bacterial species analyzed. (Resistance declined for the third bacteria, S. aureus; the researchers attribute that to strong public health efforts across Europe to reduce methicillin-resistant S. aureus, or MRSA.)
Why would temperature affect antibiotic resistance?
The researchers acknowledge that their evidence is circumstantial. In other words, both temperature and antibiotic resistance increases could have changed independently of each other. However, they lay out some potential ways that temperature could affect antibiotic resistance.
For example, in vitro experiments provide evidence that bacterial growth increases at warm temperatures, which could facilitate transmission of resistant strains. Other studies provide evidence that higher temperatures enhance transfer of antibiotic resistance genes between bacteria.
To probe the link further, the researchers call for similar long-term studies in the U.S., monitoring temperature and antibiotic resistance in different regions of the country over time.
“Our findings may motivate future research to better understand biological mechanisms or human behavior patterns, such as farming practices, that may occur in warmer locations and may have facilitated the rapid increase of antibiotic-resistant bacterial strain,” says McGough.
“A better characterization of the genetic and biological factors that may contribute to the increased spread of antibiotic-resistant strains may help us better design public health and specific clinical interventions,” adds study coauthor Derek R. MacFadden, now affiliated with the University of Ottawa.
The Canadian Institute of Health Research provided partial support for the study. Coauthors were Mohammad W. Hattab (Wyss Institute for Biologically Inspired Engineering, Harvard Medical School) and Kåre Mølbak (Statens Serum Institut, Copenhagen, Denmark).
Learn more about CHIP and its 25-year history.
Related Posts :
-

The threat from mosquito-borne diseases: Forecasting mosquitoes’ global spread
Outbreaks of mosquito-borne illnesses like yellow fever, dengue, Zika and chikungunya are rising around the world. Climate change has created ...
-

EEG markers in early life could help predict and diagnose anxiety
Anxiety disorders are the most common mental health problem among children and adolescents and are a risk factor for adult ...
-

Taming vaccine data: Joann Arce, PhD
Part of an ongoing series profiling researchers at Boston Children’s Hospital. Joann Arce, PhD, is a data tamer — corralling ...
-

Powerful new antibody neutralizes all known coronavirus variants
As the COVID-19 pandemic wears on, newer variants of the SARS-CoV-2 coronavirus have been evolving ways to evade the antibodies ...





