Two recent innovations in aerodigestive care
Feeding disorders are extremely common in pediatrics and are a source of significant stress for families. Because many complex feeding disorders lack treatment options, children tend to receive nutrition by feeding tubes as a result. The Aerodigestive Center at Boston Children’s Hospital has been at the forefront of developing novel therapies for feeding disorders. Two recent findings from the center offer clinicians and patients hope for better diagnosis and treatment of these disorders.
Treating feeding difficulties in young children: New hope from Botox?
Feeding difficulties — marked by symptoms such as retching, vomiting, and difficulty gaining weight — are common in young children, particularly those with developmental disabilities or medical complexities. Care often involves management with medication or placement of a G-tube, NG-tube, or other enteral feeding tube. These approaches have various levels of effectiveness and can result in side effects and complications.
Key takeaways:
- Complex feeding disorders can be difficult to diagnose and treat.
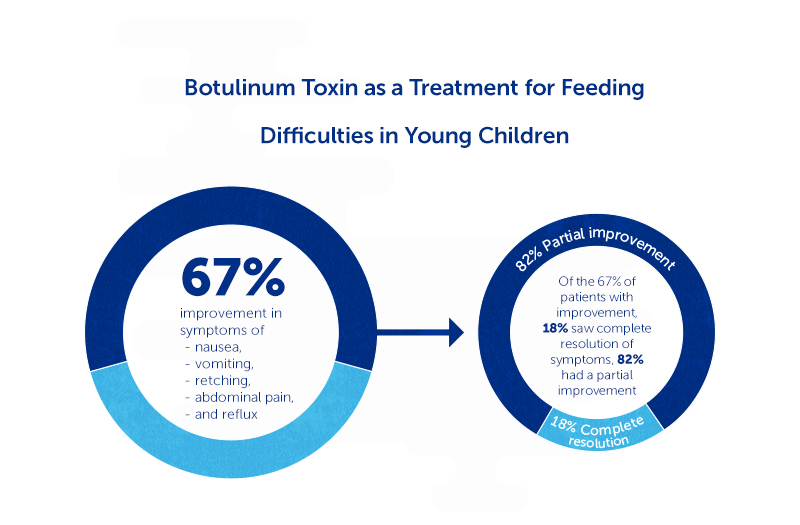
- Intrapyloric injections of botulinum toxin, or Botox, were effective at improving nausea, vomiting, retching, abdominal pain, and reflux in 67 percent of children.
- Children who have undergone surgery for GERD often continue to have problems after surgery.
- An innovative technology called functional luminal imaging probe (FLIP) may offer clinicians additional insight into these patients.
Some studies have shown intrapyloric injections of botulinum toxin (IPBI), or Botox, to be effective at reducing symptoms of nausea and vomiting in older children and adults. In this approach, botulinum toxin is injected into the pylorus, the muscle that controls stomach emptying, with the goal of relaxing the muscle or changing the sensory inputs that trigger symptoms. However, less is known about the role of IPBI in treating feeding difficulties in young children.
To learn more, Rachel Rosen, MD, MPH (director of the Aerodigestive Center), Samuel Nurko, MD, MPH (director of the Motility and Functional Gastrointestinal Disorders Center), and clinical fellow Suzanna Hirsch, MD, published data from 85 patients who had received IPBI at Boston Children’s between 2007 and 2019. The patients were all 5 years old or younger at the time of treatment, and 65 percent had an enteral tube.
The team found that 67 percent of children who received IPBI had an improvement in symptoms such as nausea, vomiting, retching, abdominal pain, and reflux. Of those patients, 82 percent had a partial improvement and 18 percent had a complete resolution of symptoms. Feeding also improved among children with enteral tubes, with more children able to feed by mouth than before receiving IPBI. The study was published in the June 26, 2020, issue of The Journal of Pediatrics.
“We have, for the first time, a treatment that offers new hope to children with feeding disorders,” says Rosen. “Vomiting and retching contribute to feeding aversions and we hope that with early treatment, we can reduce the longer-term feeding issues in these patients.”
“FLIP” for motility testing: Advanced technology sheds light on esophageal symptoms
Fundoplication is a surgical procedure that is commonly used to treat children with symptoms of gastroesophageal reflux (GERD). Children who have undergone surgery for GERD often continue to have problems after surgery, including coughing, aversion to food, poor growth, and recurrent respiratory infections. Clarifying the relationship between symptoms and testing results has been challenging. In addition, many of the current tests are difficult for the patients to tolerate, such as endoscopy, impedance testing, barium imaging, and high-resolution manometry with impedance.
An innovative technology called functional luminal imaging probe (FLIP) may offer clinicians additional insight into how distensible (stretchy) the fundoplication is in children who continue to have symptoms. That’s the finding of a recent study by Rosen, Nurko, and colleagues, which was published in the June 2020 issue of the Journal of Pediatric Gastroenterology and Nutrition.
They compared FLIP results in fundoplication patients with other patient groups to determine whether this minimally invasive catheter-based device could better assess fundoplication function over existing technology. They found that fundoplication patients had a lower distensibility of the lower esophagus compared with controls, and that a lack of stretchiness determines which children will need interventions. This lack of stretchiness places patients at risk of food refusal, lung infections, and vomiting.
“The inclusion of FLIP in our diagnostic armamentarium adds a whole new dimension to the understanding of post-operative problems in this complex population and will provide a more personalized approach to treatment,” says Nurko.
Learn more about the Aerodigestive Center and the Motility and Functional Gastrointestinal Disorders Center.
Related Posts :
-

Dysmotility may play a major role in respiratory symptoms
Clinicians whose patients exhibit respiratory symptoms frequently assume that gastroesophageal reflux disease (GERD) is responsible. However, esophageal and gastric dysmotility ...
-

Evidence-based guideline reduces G-tube placement in young patients
Gastrostomy tubes (G-tubes) are commonly used to deliver nutrition directly to the stomach in patients who cannot eat by mouth, ...
-

Study shows benefits of blended diets
Medically complex children often receive nutrition through gastrostomy tubes (G-tubes) or gastrojejunostomy tubes (G-J-tubes), frequently in the form of conventional ...
-

Better evaluation needed for BRUEs
Previously known as apparent life-threatening events, brief resolved unexplained events (BRUEs) are episodes marked by choking, paleness, blue spells (cyanosis), ...





