Botulism breakthrough? Taming botulinum toxin to deliver therapeutics
While rare, botulism can cause paralysis and is potentially fatal. It is caused by nerve-damaging toxins produced by Clostridium botulinum — the most potent toxins known. These toxins often lurk in contaminated food (home canning being a major culprit). Infants can also develop botulism from ingesting C. botulinum spores in honey, soil, or dust; the bacterium then colonizes their intestines and produces the toxin.
Key takeaway
A modified botulinum toxin efficiently targets and enters nerve cells, delivering a miniature antibody that reversed paralysis in mice.
Once paralysis develops, there is no way to reverse it, other than waiting for the toxins to wear off. People with serious cases may need to go on ventilators for weeks or months. But a new botulism treatment and delivery vehicle, described today in Science Translational Medicine, could change that.
“Currently, there are anti-toxins, but these only work before the toxins enter the motor neurons,” says Min Dong, PhD, a researcher in the Boston Children’s Hospital Department of Urology and corresponding author on the paper. “What we have developed is the first therapy that can eliminate toxins after they get inside neurons.”
If proven in humans, the approach would represent a breakthrough in treating botulism. In mice, the treatment successfully got inside neurons and reversed muscle paralysis within hours. It also enabled mice to withstand doses of botulinum toxin that would otherwise be lethal.
A botulism treatment, steered by a toxin
Dong and his colleagues needed to surmount two technical barriers that have so far thwarted effective botulism treatment. Intriguingly, their solution lay in botulinum toxin itself.
“One barrier to treatment has been getting across the cell membrane, which is difficult for protein drugs,” explains first author Shin-Ichiro Miyashita, PhD, a postdoctoral fellow in Dong’s lab. “The other is targeting specific cell types, and in this case specificity toward motor neurons and nerve terminals. We took advantage of the fact that botulinum neurotoxins naturally target motor neurons and can deliver a protein cargo across cell membranes.”
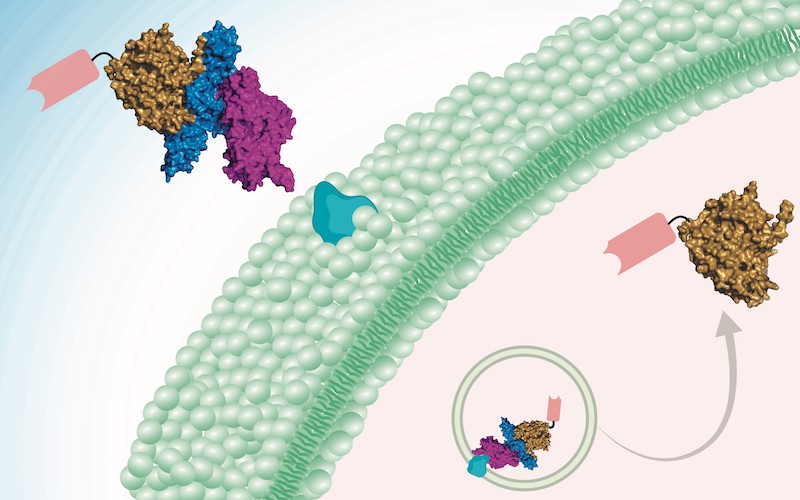
The treatment harnesses a botulinum toxin (detoxified through introduced mutations) as the delivery vehicle. The cargo — the active drug — is a mini-antibody derived from the antibodies of camels, developed by collaborator Charles Shoemaker, PhD, at Tufts University. Two of these so-called nanobodies can be delivered in tandem into neurons, neutralizing botulinum toxins type A and B at one go, the team showed.
Taming the toxin
But there was one more problem to solve.
“This approach had been attempted, but it was difficult to completely get rid of toxicity,” says Dong, “until we identified botulinum neurotoxin X in 2017. Unlike other botulinum toxins, this new toxin shows no toxicity after we introduce mutations, and serves as a safe delivery tool.”
Botox reversal
Besides botulism, Dong thinks the new treatment could be useful as a “botox reversal” agent. Botox injections, using tiny quantities of the type A botulinum toxin, can safely treat wrinkles and many other medical conditions like neck spasms, excessive sweating, or overactive bladder. However, when the injection goes awry, botox can cause unwanted muscle paralysis as a side effect, and patients have to live with the paralysis for months.
“We can potentially inject our therapeutic protein and get rid of botox in neurons and paralysis within a few hours,” Dong says.
A general delivery platform for neuroactive drugs?
The toxin-guided approach may offer a platform for getting biologic drugs into neurons to treat other disorders, Dong believes. Currently, most biologic drugs act only on cell-surface targets and cannot get into the cell’s interior.
“We provide a protein-based drug delivery platform that achieves highly specific targeting of neurons and efficient penetration of cell membranes,” Dong says. “Combined with nanobodies, which can be developed fairly readily against any protein of interest, this platform can be used to develop therapeutics that modulate proteins and biological processes inside neurons. Its modular nature even allows us to target cell types other than neurons by switching the cell-targeting domain. This could present a general approach for precision drug delivery into cells.”
Jie Zhang and Sicai Zhang of Boston Children’s Hospital and Charles Shoemaker of Tufts University are co-authors. The National Institutes of Health and Intelligence Advanced Research Projects Activity (IARPA) supported the research.
Learn more about research at Boston Children’s Hospital
Related Posts :
-

Botulism toxin X: Time to update the textbooks, thanks to genomic sequencing
Botulism is a rare, potentially fatal paralyzing illness. It’s the reason we shouldn’t feed infants honey and why ...
-

Tough yet flexible: Biologically inspired adhesive may improve fetal surgery
In children with spina bifida, the neural tube that forms the spinal cord and brain doesn’t close during early ...
-

Precision chemo-immunotherapy for pancreatic cancer?
Pancreatic cancer is highly lethal and in great need of better treatments. Only about 10 percent of patients remain alive five ...
-

From ‘hit to vial’: Discovery and optimization of a promising vaccine adjuvant
Many vaccines are only partially effective, have waning efficacy, or do not work well in the very young or the ...





