More details on MIS-C, the post-COVID multi-system inflammatory syndrome in children

Boston Children’s Hospital and collaborators launched the national Overcoming COVID-19 study in April to track children, teens, and young adults hospitalized with COVID-19 across the U.S. In yesterday’s New England Journal of Medicine, investigators provides a fuller picture of the still-mysterious, life-threatening multi-system inflammatory syndrome in children (MIS-C).
· The largest case series of MIS-C to date refines previous descriptions and highlights cardiovascular complications.
· The study is continuing to track MIS-C cases across the U.S.
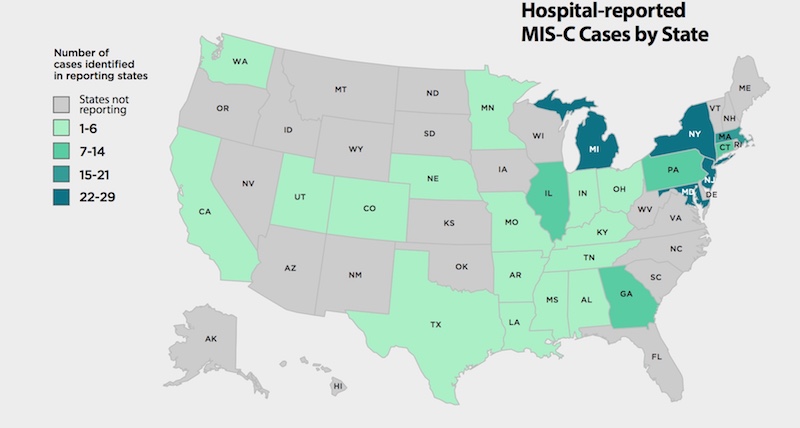
The report describes 186 children and adolescents diagnosed with MIS-C from March 15 to May 20, 2020 — the largest published case series to date. In all, 53 pediatric hospitals from 26 states reported cases. The study continues to track U.S. cases as COVID-19 unfolds.
Cardiovascular symptoms in MIS-C call for close monitoring
The new study highlights a high rate of cardiovascular symptoms in MIS-C — affecting 80 percent of patients — and involvement of the coronary arteries that can potentially lead to deadly aneurysms.
“The proportion with involvement of the coronary arteries was 8 percent, says Adrienne Randolph, MD, of Boston Children’s, the study’s lead investigator. “That included patients who did not meet many of the criteria for Kawasaki disease.” (Kawasaki is a rare syndrome causing blood-vessel inflammation that has been described as part of MIS-C.)
“Our findings point out the need for serial echocardiograms to monitor the heart and coronary arteries of children with MIS-C,” says Randolph. “They also prove how important real-time surveillance is during a pandemic.”
MIS-C demographics
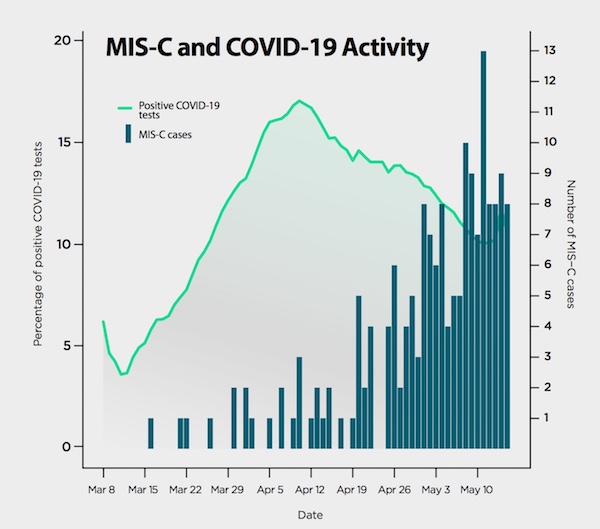
Nearly 90 percent of patients were hospitalized after April 16, generally following a local peak in COVID-19 cases. This fits the pattern of a delayed, post-COVID syndrome. Seventy percent of patients tested positive for the virus or antibodies to it. The rest had a documented exposure to someone with COVID-19.
Fully 73 percent of patients were previously healthy. Their median age was 8.3 years, and there were slightly more males (62 percent). Twenty-five percent were Black, 31 percent were Hispanic or Latino, and 19 percent were White. The remaining 27 percent were “other” or of unknown race.
Patients with MIS-C spent an average of one week in the hospital, and 79 percent needed intensive care. Four children (2 percent) died, two of whom were previously healthy.
Defining MIS-C: Inflammation, multi-organ involvement
Inflammation and fever were defining features of MIS-C. All patients had fever (lasting a median of six days), and 92 percent had four or more biomarkers indicating inflammation.
Multiple organs were affected: 71 percent had involvement of four or more organ systems:
- 92 percent had gastrointestinal involvement (nausea, vomiting, diarrhea, abdominal pain).
- 80 percent had cardiovascular involvement, including heart arrhythmias, weakened heartbeats, inflammation around the heart, and need for CPR. Eight percent of all patients had documented coronary artery aneurysms, and 48 percent needed treatment to improve heart function and blood pressure. Cardiovascular involvement was most common in older children and young adults.
- 76 percent had blood abnormalities, including abnormal blood cell counts, deep vein thrombosis and pulmonary embolism; 47 percent received treatment to prevent clots.
- 74 percent had involvement of the mucous membranes and skin, affecting the mouth, eyes, hands and feet.
- 70 percent had respiratory symptoms; 20 percent needed mechanical ventilation and another 17 percent received non-invasive ventilation.
More than a third of patients had features that overlap with Kawasaki disease. But the investigators note that 60 percent would not have met criteria for Kawasaki disease or even “incomplete” Kawasaki disease.
See more data from the study in this infographic from the CDC.
More coverage of MIS-C and COVID-19 research at Boston Children’s Hospital
Future plans
The Overcoming COVID-19 study will continue to track children and youth hospitalized with COVID-19, aiming for a total of 1,000 patients at more than 70 pediatric centers. About half of the patients will have detailed, prospective observation and periodic collection of respiratory and blood samples. These will be used to investigate a variety of parameters, including markers of immune response and inflammation and the effects of various treatments used for COVID-19.
“We need to understand the full spectrum of COVID-19 and MIS-C in children and young adults,” says Randolph. “We need to know why certain children and adults are so susceptible while others are not, and what their long-term outcomes are.”
Manish M. Patel, MD, of the Centers for Disease Control and Prevention was co-senior investigator on the study. Leora R. Feldstein, PhD, MSc, and Erica Billig Rose PhD, MS, of CDC were co-first authors on the paper.
Learn more about the hospital’s response to COVID-19.
Related Posts :
-

Building better antibodies, curbing autoimmunity: New insights on B cells
When we’re vaccinated or exposed to an infection, our B cells spring into action, churning out antibodies that are ...
-

Could SIDS be caused by unrecognized brain infections?
Some infants who pass away from sudden infant death syndrome (SIDS) are known to have had acute minor infections. Could ...
-

Could a GI bug’s toxin curb hard-to-treat breast cancer?
Clostridium difficile can cause devastating inflammatory gastrointestinal infections, with much of the damage inflicted by a toxin the bug produces. ...
-

A new approach to C. diff? Targeting the inflammation, not the bacteria
Clostridium difficile (C. diff) intestinal infections can cause severe, debilitating diarrhea in patients who are hospitalized or on immunosuppressive therapies. ...





