Scoliosis patients get a preview of spinal fusion surgery

“Patients are more at ease when they know what to expect,” says, Dr. Daniel Hedequist, chief of the Spine Division in the Department of Orthopedic Surgery. Dr. Hedequist performs dozens of spinal fusion surgeries each year to treat children with scoliosis. While the procedure is familiar ground for the surgical team at Boston Children’s Hospital, it’s unknown territory for most patients and their families.
“I kept hearing from parents whose children were scheduled for surgery that their children felt totally out of control,” says Dr. Hedequist. With patients like this in mind, clinicians in the Spine Division teamed up with Brianna O’Connell, the Simulation Program’s child life specialist, to create an immersive experience for patients and their families before they have surgery.
Spinal fusion surgery, step by step
The simulation program includes realistic set ups of pre-op, the operating room, recovery room, and an inpatient hospital room. Patients and families have a chance to see medical equipment up close and meet members of the surgical team, many of whom will care for them during their stay at Boston Children’s. They also have the chance to ask questions about any aspect of spinal fusion surgery and what to expect when they return home.
“The simulation lab is a great opportunity to acquaint kids with what they will see and experience on surgery day,” says O’Connell who runs programs for patients and caregivers at the Boston Children’s SIMPeds Simulator Program. “They get to take a close look at the equipment and talk with their surgical team in a non-threatening environment.”
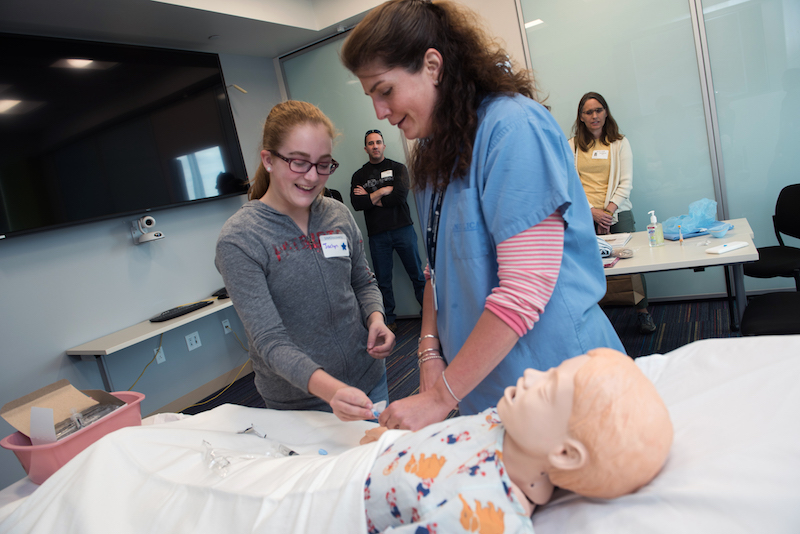
Pre-op holding area
At their first stop, patients learned what to expect on the morning of their surgery, starting with the pain-free IV system. A burst of topical anesthetic will numb the skin and then a very thin, soft, flexible IV will be inserted into a vein in the arm. For patients who don’t like needles, the pre-op team suggested a number of relaxation techniques, including deep breathing exercises, listening to music, or watching a YouTube video. Here, a patient helps give a mannequin medicine intravenously.
Operating room
Next, patients entered a simulated operating room. At this station, patients learned about the different monitors the surgical team uses during surgery and what to expect when they are given anesthesia. The patient will fall asleep while a group of caregivers takes care of them. Once asleep, the patient will be gently rolled onto their stomach. A surgical drape will be placed over them so that only an area of their back is exposed during surgery.

Surgical hardware
Titanium rods and screws will be used to straighten and stabilize the patient’s spine. Here, Dr. Hedequist uses a spinal model to demonstrate the hardware that will hold a section of the spine in a straight position while the vertebrae heal into a solid, stable bone. Typically, this takes six months to a year. After spinal fusion surgery, many patients grow taller.

Surgical team
In addition to the surgeon and anesthesiologist, many assistants and nurses help ensure the surgery goes smoothly. This team closely monitors the patient’s neurological activity throughout the procedure to make sure manipulating the spine does not have any adverse impact on motor skills. Here, a nurse explains who the members of the surgical team are and what they do.

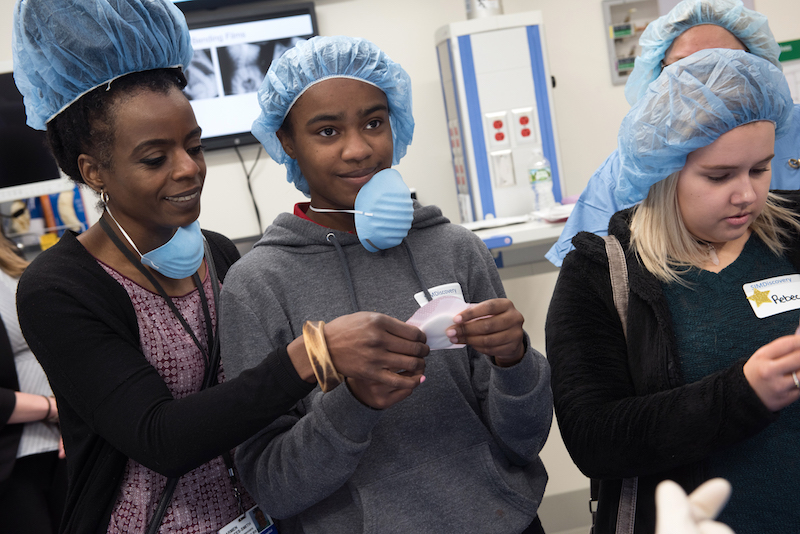
Surgical padding
Patients and their families got to see some of the equipment and materials that will be used during surgery. Here, they test out samples of the soft padding that pads patients’ knees and hip bones during the procedure.
Surgical equipment
The surgical table for spinal fusion is a special, adjustable surface that cradles patients’ bodies during surgery. Here, a nurse presses on the table’s cushiony material, demonstrating how supportive it is.

Recovery room
After waking up from anesthesia, patients can expect to be a bit disoriented. They will be wearing an oxygen mask like the one in the picture below. The patient’s parents be with them in the recovery room when they first wake up, or will arrive soon.

Inpatient room
After recovery, the patient will be brought to their hospital room in the 10 Northwest wing of Boston Children’s. They will remain there for the next few days until they are ready to go home. Here, a nurse practitioner uses a medical mannequin to show patients the type of bandage used to protect the surgical incision.

Vital signs and pain management
During their stay at the hospital, the patient will receive round-the-clock care with nurses periodically checking their vital signs. Below, a patient tries out a stethoscope to see if she can find a pulse on a medical mannequin. This hi-fidelity mannequin has a pulse, heartbeat, and lung sounds.

The first day after surgery, the patient will be able to manage their pain by pushing a button that releases painkillers through their IV line. As soon as they can take food and drink by mouth, they will be switched to oral painkillers.
Physical therapy
Physical therapy is an essential part of spinal fusion surgery. After the procedure, a physical therapist will help the patient reach milestones like walking down the hallway and using the bathroom on their own. These are part of a checklist of things a patient must be able to do before they can go home. The “log roll,” demonstrated below, is a technique for getting out of the bed without bending or twisting the spine.

One year after spinal fusion surgery
A patient who had spinal fusion surgery at Boston Children’s the previous year attended the simulation program and answered questions about her experience. One patient asked how long it was before she was able to be active again after surgery. While recovery is different for each person, this patient (below, right) was gradually able to become more active as her spine healed. Today, a year after surgery, she is back to running cross country and doing all the things she did before having surgery.

In control of their health
“Providing developmentally appropriate information before surgery helps patients feel more in control of their own health and well-being,” says Erin Whooley, child life specialist in the Perioperative Care Coordination Clinic. “Since we first started offering this program in 2017, we’ve found that the procedure is more predictable for patients and they feel more in control.”
Simulation days are typically scheduled around school breaks, so kids don’t have to miss school. In 2019, spinal fusion simulation days took place in March, April, and June. “This is for patients and their parents, so we do everything we can to accommodate their schedules,” says O’Connell.
For more information about the simulation program, contact Brianna O’Connell at Brianna.OConnell@childrens.harvard.edu.
Learn more about the Spine Division.
Related Posts :
-

Ask a sports medicine specialist: Why are ACL tears so common among female athletes?
When an athlete is sprinting after an opponent who suddenly stops or changes direction, their anterior cruciate ligaments (ACLs) make ...
-

Forging a path back to school after orthopedic trauma
Orthopedic trauma can force children to miss school, sometimes for an extended period. But even when patients have regained enough ...
-

Jackie’s dreams of playing professional soccer back on track after ACL surgery
From her dorm in Newcastle, England, Jackie Zapata can hear fans roaring in the soccer stadium a few blocks away. ...
-

What orthopedic trauma surgeons wish more parents knew about lawnmower injuries
Summer is full of delights: lemonade, ice cream, and fresh-cut grass to name a few. Unfortunately, the warmer months can ...





