To monitor health, simply trip the ‘nanoswitches’
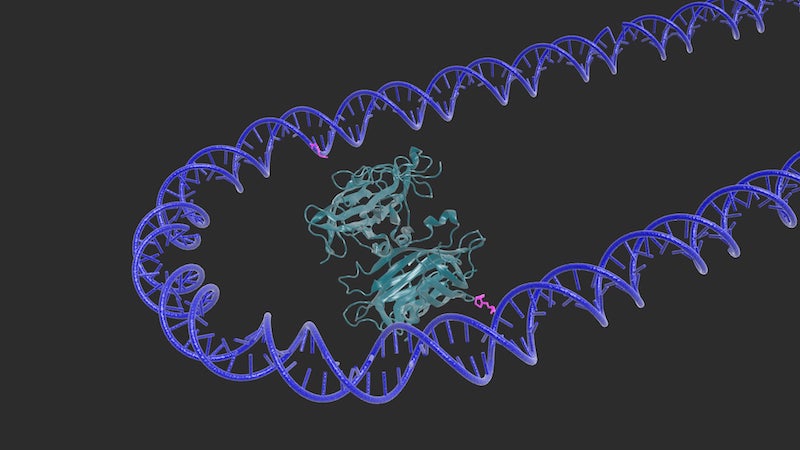
“Nanoswitches” — engineered, shape-changing strands of DNA — could shake up the way we monitor our health, according to new research. Faster, easier, cheaper and more sensitive tests based on these tools — used in the lab or at point of care — could indicate the presence of disease, infection and even genetic variabilities as subtle as a single-gene mutation.
“One critical application in both basic research and clinical practice is the detection of biomarkers in our bodies, which convey vital information about our current health,” says lead researcher Wesley Wong, PhD, of Boston Children’s Hospital Program in Cellular and Molecular Medicine (PCMM). “However, current methods tend to be either cheap and easy or highly sensitive, but generally not both.”
That’s why Wong and his team have adapted their DNA nanoswitch technology — previously demonstrated to aid drug discovery and the measure of biochemical interactions — into a new platform that they call the nanoswitch-linked immunosorbent assay (NLISA) for fast, sensitive and specific protein detection. It’s described this week in the Proceedings of the National Academy of Sciences.
“It’s a ‘best of both worlds’ approach,” says Wong, senior author on the paper, who is also an assistant professor at Harvard Medical School and an associate faculty member at Harvard University’s Wyss Institute for Biologically Inspired Engineering. “This technology could translate into laboratory and point-of-care tests that are as affordable and easy to use as at-home pregnancy tests, but are much more sensitive and accurate.”
The NLISA platform uses a standard laboratory process called gel electrophoresis to screen synthesized, single strands of DNA “reagents” that are programmed to change their shape in the presence of a specific biomarker. They begin as long, linear strands of DNA, but are decorated with proteins that will bind to a matching protein biomarker of interest. Once exposed to that matching biomarker, the proteins bind to it and cause the DNA strand to bend into a loop.
‘Run the gel’
When combined with gel electrophoresis, that shape change makes it extremely easy to detect whether or not the biomarker of interest is present. In gel electrophoresis, an electric field pulls molecules through a porous gel. Linear, un-activated DNA nanoswitches move much faster through the gel, while triggered nanoswitch loops move much slower because of their clunkier shape.
“Simply put, the distances the nanoswitches travel through the gel indicate whether a biomarker is present or not,” says first author Clinton Hansen, PhD, a postdoctoral fellow in the Wong lab.
Take, for example, prostate-specific antigen (PSA), a blood serum marker used to test men for prostate cancer. To demonstrate their NLISA system, Wong and his team spiked serum samples with varied levels of PSA, combined them with the nanoswitch reagents for PSA and performed gel electrophoresis on the mixture. The team was able to detect PSA with higher sensitivity using less blood serum than comparable assays.
During another proof-of-concept demonstration, Wong’s team showed that their NLISA platform could distinguish between highly similar viral strains of dengue fever in 45 minutes or less.
“By running a gel, we perturb the nanoswitches with an electric field to reduce false-positive results using a process called ‘kinetic proofreading,’” Wong explains. “Although similar proteins — such as related viral strains — might initially ‘trip’ the nanoswitches into loops, these close-but-not-quite-perfect bonds can be broken, leaving behind only true positive results. This allows us to discern between viral strains that may even be different by just a single gene mutation.”
The NLISA system has the potential to become a standard for protein detection, Wong suggests, and could even be developed into a portable, handheld device for clinical use.
##
In addition to Wong and Hansen, additional authors of the new study are Darren Yang (Boston Children’s) and Mounir Koussa (HMS).
Funding for this work was provided by the Boston Children’s Technology Development Fund, the Harvard Blavatnik Biomedical Accelerator, the Wyss Institute, the Arnold and Mabel Beckman Foundation Young Investigator 683 Award and the National Institutes of Health (National Institute of General 684 Medical Sciences Grant R35 GM119537 and National Cancer Institute Grant Q:16 685 R21 CA212827).
More research from Boston Children’s PCMM…
Related Posts :
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Modeling urinary tract disorders on a chip: Zohreh Izadifar
When a new tissue sample arrives from the Department of Urology, the Boston Children’s Hospital lab of Zohreh Izadifar, ...
-

Bringing order to disorder: Jhullian Alston, PhD
Proteins typically fold into orderly, predictable three-dimensional structures that dictate how they will interact with other molecules. Jhulian Alston, PhD, ...
-

Changing lives through genetics: The Children’s Rare Disease Collaborative
A 14-year-old girl was having back pain after a car accident and visited an orthopedic clinic at Boston Children’s ...